Calcaneal Apophysitis In Youngsters
During a growth spurt, your child?s heel bone grows faster than the muscles, tendons, and ligaments in her leg. In fact, the heel is one of your child?s first body parts to reach full adult size. When the muscles and tendons can?t grow fast enough to keep up, they are stretched too tight. If your child is very active, especially if she plays a sport that involves a lot of running and jumping on hard surfaces (such as soccer, basketball, or gymnastics), it can put extra strain on her already overstretched tendons. This leads to swelling and pain at the point where the tendons attach to the growing part of her heel.
Causes
This condition is more common in boys than girls. It generally presents between the ages of 9-14 and peaks between ages 10-12 years. This injury can reoccur up until the age of 17, when the growth plate of the calcaneous generally closes. These types of injuries will commonly occur during periods of rapid growth. Sever?s Disease occurs more frequently in child with flat feet, but all children with flat feet will not get Sever?s.
Symptoms
The most obvious sign of Sever's disease is pain or tenderness in one or both heels, usually at the back. The pain also might extend to the sides and bottom of the heel, ending near the arch of the foot. A child also may have these related problems, swelling and redness in the heel, difficulty walking, discomfort or stiffness in the feet upon awaking, discomfort when the heel is squeezed on both sides, an unusual walk, such as walking with a limp or on tiptoes to avoid putting pressure on the heel. Symptoms are usually worse during or after activity and get better with rest.
Diagnosis
Children or adolescents who are experiencing pain and discomfort in their feet should be evaluated by a physician. In some cases, no imaging tests are needed to diagnose Sever?s disease. A podiatrist or other healthcare professional may choose to order an x-ray or imaging study, however, to ensure that there is no other cause for the pain, such as a fracture. Sever?s disease will not show any findings on an x-ray because it affects cartilage.
Non Surgical Treatment
The immediate goal of treatment is pain relief. Because symptoms generally worsen with activity, the main treatment for Sever's disease is rest, which helps to relieve pressure on the heel bone, decreasing swelling and reducing pain. As directed by the doctor, a child should cut down on or avoid all activities that cause pain until all symptoms are gone, especially running barefoot or on hard surfaces because hard impact on the feet can worsen pain and inflammation. The child might be able to do things that do not put pressure on the heel, such as swimming and biking, but check with a doctor first.
Exercise
The following exercises are commonly prescribed to patients with Severs disease. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 1 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Calf Stretch with Towel. Begin this exercise with a resistance band around your foot and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free. Once you can perform 20 repetitions consistently without pain, the exercise can be progressed by gradually increasing the resistance of the band provided there is no increase in symptoms. Bridging. Begin this exercise lying on your back in the position demonstrated. Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds then slowly lower your bottom back down. Repeat 10 times provided the exercise is pain free.
Causes Of Acquired Flat Foot
Overview
Adult acquired flatfoot is one of the most common problems affecting the foot and ankle. Treatment ranges from nonsurgical methods, such as orthotics and braces to surgery. Your doctor will create a treatment plan for you based on what is causing your AAFD. 
Causes
There are a number of theories as to why the tendon becomes inflamed and stops working. It may be related to the poor blood supply within the tendon. Increasing age, inflammatory arthritis, diabetes and obesity have been found to be causes.
Symptoms
Pain and swelling around the inside aspect of the ankle initially. Later, the arch of the foot may fall (foot becomes flat), this change leads to walking to become difficult and painful, as well as standing for long periods. As the flat foot becomes established, pain may progress to the outer part of the ankle. Eventually, arthritis may develop.
Diagnosis
Observe forefoot to hindfoot alignment. Do this with the patient sitting and the heel in neutral, and also with the patient standing. I like to put blocks under the forefoot with the heel in neutral to see how much forefoot correction is necessary to help hold the hindfoot position. One last note is to check all joints for stiffness. In cases of prolonged PTTD or coalition, rigid deformity is present and one must carefully check the joints of the midfoot and hindfoot for stiffness and arthritis in the surgical pre-planning.
Non surgical Treatment
Nonoperative treatment of stage 1 and 2 acquired adult flatfoot deformity can be successful. General components of the treatment include the use of comfort shoes. Activity modification to avoid exacerbating activities. Weight loss if indicated. Specific components of treatment that over time can lead to marked improvement in symptoms include a high repetition, low resistance strengthening program. Appropriate bracing or a medial longitudinal arch support. If the posterior tibial tendon is intact, a series of exercises aimed at strengthening the elongated and dysfunctional tendon complex can be successful. In stage 2 deformities, this is combined with an ankle brace for a period of 2-3 months until the symptoms resolve. At this point, the patient is transitioned to an orthotic insert which may help to support the arch. In patients with stage 1 deformity it may be possible to use an arch support immediately. 
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Pain In The Foot's Arch Triggers Signs And Symptoms And Treatment Options
The plantar fascia is a sturdy structure but the degree of stress that it takes makes it susceptible to injury. A force equal to almost three times body weight passes through the foot with each step. On running, this typically happens about 90 times a minute. Plantar fasciitis is thought to be a traction and overuse injury. Damage to the plantar fascia is usually in the form of micro-tears. It is a degenerative rather than an inflammatory process. Damage tends to occur near the heel, where stress on the fibres is greatest, and where the fascia is the thinnest. The fascia broadens as it extends toward the toes.
Plantar fasciitis is often associated with calcaneal spurs. These are depositions of calcium where the fascia suffers most damage. Spurs are most commonly on the medial side at the origin of the fascia from the calcaneum. Spurs are the result of the process of plantar fasciitis and not the cause of the pain. It can present bilaterally.

Causes
Also known as pes planus, this is when the arch of the foot collapses completely dropping the whole sole of the foot down to the ground. Flat feet are a common cause of foot arch pain. Babies are born with flat feet and as they grow, the foot arches should gradually form, but in approximately 30% of the population, they never do. They can also develop later in life, due to illness, pregnancy, injury, excessive stress on the feet or as part of the aging process. Many people who have flat feet don?t complain of any accompanying symptoms, but some develop foot arch pain, or problems further up the leg such as knee pain or back pain. They may find their feet tire quickly when they are standing or walking, and that it is difficult to rise up onto their tiptoes. Someone who is experiencing pain on the bottom of the foot or elsewhere due to their flat feet can benefit from exercises and orthotics (specially designed insoles to correct the foot position) as well as walking barefoot rather than in shoes. A quick test to see if you have flat feet is to put your foot in a tray of water and then place it on a smooth level surface e.g. thick paper. Have a look at your footprint, the more of the sole of the foot that you can see, the flatter your foot.
Symptoms
The foot of a newborn with congenital vertical talus typically has a convex rocker-bottom shape. This is sometimes combined with an actual fold in the middle of the foot. The rare person who is diagnosed at an older age often has a "peg-leg" gait, poor balance and heavy calluses on the soles where the arch would normally be. If a child with congenital vertical talus has a genetic disorder, additional symptoms often are seen in other parts of the body.
Diagnosis
In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics.
Non Surgical Treatment
The treatment of a rigid flatfoot depends on its cause. Congenital vertical talus. Your doctor may suggest a trial of serial casting. The foot is placed in a cast and the cast is changed frequently to reposition the foot gradually. However, this generally has a low success rate. Most people ultimately need surgery to correct the problem. Tarsal coalition. Treatment depends on your age, extent of bone fusion and severity of symptoms. For milder cases, your doctor may recommend nonsurgical treatment with shoe inserts, wrapping of the foot with supportive straps or temporarily immobilizing the foot in a cast. For more severe cases, surgery is necessary to relieve pain and improve the flexibility of the foot. Lateral subtalar dislocation. The goal is to move the dislocated bone back into place as soon as possible. If there is no open wound, the doctor may push the bone back into proper alignment without making an incision. Anesthesia is usually given before this treatment. Once this is accomplished, a short leg cast must be worn for about four weeks to help stabilize the joint permanently. About 15% to 20% of people with lateral subtalar dislocation must be treated with surgery to reposition the dislocated bone.

Surgical Treatment
Surgical advances have dramatically improved the ability to alleviate the pain and decreased function that millions of Americans experience due to flat feet. Nevertheless, many patients and even some physicians remain unaware of the new procedures, which are best performed by a foot and ankle specialist who has the applicable training and experience.
Prevention
The best method for preventing plantar fasciitis is stretching. The plantar fascia can be stretched by grabbing the toes, pulling the foot upward and holding for 15 seconds. To stretch the calf muscles, place hands on a wall and drop affected leg back into a lunge step while keeping the heel of the back leg down. Keep the back knee straight for one stretch and then bend the knee slightly to stretch a deeper muscle in the calf. Hold stretch for 15 seconds and repeat three times.
What'S Adult Aquired FlatFoot ?
Overview
Adult acquired flatfoot deformity (AAFD) is a painful, chronic condition found most often in women between the ages of 40 and 60. AAFD occurs when the soft tissues of the foot are overstretched and torn, causing the arch to collapse. Flatfoot deformities may also be caused by a foot fracture, or may result from long-term arthritis. Once the posterior tibial tendon-the tendon unit that holds up the arch-loses its function, the foot becomes ?flat? as the bones spread out of position during weight bearing. Without an AAFD repair, the condition may progress until the affected foot becomes entirely rigid and quite painful. 
Causes
The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
Observation by a skilled foot clinician and a hands-on evaluation of the foot and ankle is the most accurate diagnostic technique. Your Dallas foot doctor may have you do a walking examination (the most reliable way to check for the deformity). During walking, the affected foot appears more pronated and deformed. Your podiatrist may do muscle testing to look for strength deficiencies. During a single foot raise test, the foot doctor will ask you to rise up on the tip of your toes while keeping your unaffected foot off the ground. If your posterior tendon has been attenuated or ruptured, you will be unable to lift your heel off the floor. In less severe cases, it is possible to rise onto your toes, but your heel will not invert normally. X-rays are not always helpful as a diagnostic tool for Adult Flatfoot because both feet will generally demonstrate a deformity. MRI (magnetic resonance imaging) may show tendon injury and inflammation, but can?t always be relied on for a complete diagnosis. In most cases, a MRI is not necessary to diagnose a posterior tibial tendon injury. An ultrasound may also be used to confirm the deformity, but is usually not required for an initial diagnosis.
Non surgical Treatment
A painless flatfoot that does not hinder your ability to walk or wear shoes requires no special treatment or orthotic device. Other treatment options depend on the cause and progression of the flatfoot. Conservative treatment options include making shoe modifications. Using orthotic devices such as arch supports and custom-made orthoses. Taking nonsteroidal anti-inflammatory drugs such as ibuprofen to relieve pain. Using a short-leg walking cast or wearing a brace. Injecting a corticosteroid into the joint to relieve pain. Rest and ice. Physical therapy. In some cases, surgery may be needed to correct the problem. Surgical procedures can help reduce pain and improve bone alignment. 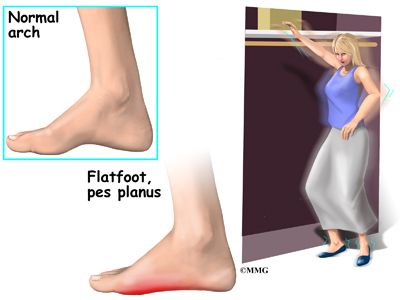
Surgical Treatment
For more chronic flatfoot pain, surgical intervention may be the best option. Barring other serious medical ailments, surgery is a good alternative for patients with a serious problem. There are two surgical options depending on a person?s physical condition, age and lifestyle. The first type of surgery involves repair of the PTT by transferring of a nearby tendon to help re-establish an arch and straighten out the foot. After this surgery, patients wear a non-weight bearing support boot for four to six weeks. The other surgery involves fusing of two or three bones in the hind foot below the ankle. While providing significant pain relief, this option does take away some hind foot side-to-side motion. Following surgery, patients are in a cast for three months. Surgery is an effective treatment to address adult-acquired flatfoot, but it can sometimes be avoided if foot issues are resolved early. That is why it is so important to seek help right away if you are feeling ankle pain. But perhaps the best way to keep from becoming flatfooted is to avoid the risk factors altogether. This means keeping your blood pressure, weight and diabetes in check.
Tips To Manage Pes Planus

Flatfoot (pes planus) is a condition that occurs when the arch or instep of the foot collapses or touches the standing surface. It is also known as fallen arches or pronation of the feet. The human foot is made up of 26 bones, 33 joints, and over 100 muscles, tendons and ligaments. The arch of the foot is created by tightening of the muscles and various ligaments that support the bones of the arch as well as ligaments that run from the heel to the ball of the foot. The arches distribute weight evenly across the feet and up the legs, and can affect walking. A well-developed arch is balanced between rigidity (for stability) and flexibility (for adapting to surfaces).
Causes
Genetic predisposition. Faulty foot mechanics, e.g. excessive pronation. Abnormal bony architecture. Laxity of ligaments. Neuro-muscular disease. Trauma to the leg muscles or major tendons. Inflammatory diseases of the joints e.g. Rheumatoid arthritis. Surgical procedures on the leg and ankle. Limb length inequality. Tight Achilles tendon.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Your doctor will ask about your symptoms and medical history. A physical and foot exam will be done. Flat feet can be diagnosed by appearance. To determine if the foot is rigid, you may be asked to do some simple tasks.
Non Surgical Treatment
Most cases of fallen arches are not painful and need no form of treatment. However, common symptoms of fallen arches can include pain in your feet (particularly in the area of your heel or arch), pain in your feet that persists after long bouts of physical activity or standing up, achy feet, or arch pain when standing on the tips of your toes. Most cases of fallen arches are not preventable. Treatments for fallen arches include, rest, ice, compression, medication to relieve pain, orthotics, or in some cases surgery.
Surgical Treatment

A combination of surgical procedures can be used to reconstruct the flatfoot. Generally, these procedures can be separated into those that correct deformities of the bones and those that repair ligaments and tendons. Your orthopaedic surgeon will choose the proper combination of procedures for your foot. Surgery of the foot can be performed under regional anesthesia, which is numbing the foot and ankle with a nerve or spinal block, or general anesthesia, which may require a breathing tube. A nerve block is often placed behind the knee to reduce pain after surgery.
Prevention
Flat feet or Fallen Arches cannot be prevented due to congenital of nature or from underlying disease process; however, painful symptoms and future pathology from Flat Feet or Fallen Arches may be prevented by the following. Continue to wear your orthotics for work and exercise to provide stability and maintain function of your feet. Footwear. Continue to wear supportive shoes to maximise the function of your orthotic and prevent excessive movement of the joints in your feet.
Bunions Everything You Need To Learn

A bunion is a bony bump on the joint at the base of your big toe. The bony growth on the joint sometimes causes your big toe to Bunion Surgery at Nuffield Health Hospitalsturn in towards your second toe. Symptoms include pain, swelling of your big toe and, as the bunion sticks out, it can often rub on the inside of your shoe. The cause is not always known, there may be a deformity of the joint, called hallux valgus (hallux means big toe, valgus means bent outwards). Or it can be as simple as ill fitting footwear not allowing enough width to fit the toes in their natural position. Sometimes bunions are associated with arthritis in the joint at the base of your big toe. Left untreated bunions can continue to grow and become more painful.
Causes
The underlying cause is a deformity of the joint at the base of the big toe. The deformity is called hallux valgus. In this deformity the joint develops a prominent sideways angle. Due to this deformity the bones of the big toe are pushed towards the smaller toes. The skin over the angled joint then tends to rub on the inside of shoes. This may cause thickening and inflammation of the overlying skin and tissues next to the affected joint. In most cases it is not clear why a hallux valgus deformity develops. There may be some hereditary (genetic) tendency to have a weakness of this joint. In some cases it is associated with a joint problem such as osteoarthritis or rheumatoid arthritis. However, whatever the underlying cause, wearing tight or badly fitting shoes tends to make the problem worse. Wearing such shoes puts extra pressure on the big toe joint and causes friction on the overlying skin.
Symptoms
The main problem is usually the pressure of the shoe over the bony prominence, which causes discomfort or pain. Sometimes the skin over the lump becomes red, blistered or infected. The foot may become so broad that it is difficult to get wide enough shoes. The big toe sometimes tilts over so much that it rubs on the second toe, or pushes it up out of place so it presses on the shoe. Also, the big toe does not work as well with a bunion, and the other toes have to take more of the weight of the body as you walk. This can cause pain under the ball of the foot ("metatarsalgia"). Sometimes arthritis develops in the deformed joint, causing pain in the joint.
Diagnosis
Your doctor can identify a bunion by examining your foot. Watching your big toe as you move it up and down will help your doctor determine if your range of motion is limited. Your doctor will also look for redness or swelling. After the physical exam, an X-ray of your foot can help your doctor identify the cause of the bunion and rate its severity.
Non Surgical Treatment
Wear comfortable shoes that don't squeeze your toes together. Sandals are ideal in warm weather. Cushioning the bunion with a donut-shaped bunion pad sold at drugstores can prevent any direct rubbing against your shoes. Have your shoes stretched to give your foot more room or consider switching to footwear customized to relieve pressure on the affected area. Soak your foot in warm water to help lessen the pain after a day on your feet. Apply ice packs several times a day to reduce swelling of painful and inflamed bunions. Take aspirin or ibuprofen for the inflammation and pain, and try supplementing with anti-inflammatory herbs such as ginger and turmeric (these work more slowly than the drugs). See a podiatrist for specially fitted shoes or orthotic devices that may help. Sometimes, surgery is necessary. Seek a second opinion before scheduling any operation.

Surgical Treatment
As mentioned above, with mild cases, the bone is cut close to the big toe joint and shifted over into a correct position. The cut bone is held in placed with one or two surgical screws. With this procedure, just the top of the bone is moved over and the bottom of the bone remains in the same place. This technique is called the Austin bunionectomy and refers to type of bone cut that will be made by the Surgeon. There is, however, a limit on how far one can move the bone over with this technique. Its is generally thought that the cut bone should only be moved over a distance equal to half the width of the bone. In somes the bone may be moved over further.
All You Want To Find Out Related To Pain In The Arches
The most common causes of arch pain are repetitive activities, such as walking or running too far; jumping; or standing on hard surfaces for long periods of time. Injury, such as tears in the ligament called the plantar fascia. The natural aging process. Biomechanical defects of the foot, or abnormalities we are born with, such as very high or low arches, or pronation (a turning out of the foot, causing us to walk more on the inner border of the foot). Plantar fibromatosis, a benign growth on the ligament that supports the arch.

Causes
The plantar fascia is designed to absorb the high stresses and strains we place on our feet. But, sometimes, too much pressure damages or tears the tissues. The body's natural response to injury is inflammation, which results in the heel pain and stiffness of plantar fasciitis.
Symptoms
The primary symptom is pain or aching in the arch area. This can be accompanied by inflammation and tenderness. If the pain is caused by the plantar fascia, it is likely to be considerably more severe in the mornings due to the muscles being unused.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
Flat feet in a child do not need treatment if they are not causing pain or walking problems. Your child's feet will grow and develop the same, whether special shoes, shoe inserts, heel cups, or wedges are used. Your child may walk barefoot, run or jump, or do any other activity without making the flat feet worse. In older children and adults, flexible flat feet that do not cause pain or walking problems do not need further treatment. If you have pain due to flexible flat feet, the following may help. An arch-support (orthotic) that you put in your shoe. You can buy this at the store or have it custom-made. Special shoes. Rigid or painful flat feet need to be checked by a health care provider. The treatment depends on the cause of the flat feet. For tarsal coalition, treatment starts with rest and possibly a cast. Surgery may be needed if pain does not improve. In more severe cases, surgery may be needed to clean or repair the tendon, fuse joints in the foot into a corrected position. Flat feet in older adults can be treated with pain relievers, orthotics, and sometimes surgery.

Surgical Treatment
Surgery for flat feet is separated into three kinds: soft tissue procedures, bone cuts, and bone fusions. Depending on the severity of the flat foot, a person?s age, and whether or not the foot is stiff determines just how the foot can be fixed. In most cases a combination of procedures are performed. With flexible flat feet, surgery is geared at maintaining the motion of the foot and recreating the arch. Commonly this may involve tendon repairs along the inside of the foot to reinforce the main tendon that lifts the arch. When the bone collapse is significant, bone procedures are included to physically rebuild the arch, and realign the heel. The presence of bunions with flat feet is often contributing to the collapse and in most situations requires correction. With rigid flat feet, surgery is focused on restoring the shape of the foot through procedures that eliminate motion. In this case, motion does not exist pre-operatively, so realigning the foot is of utmost importance. The exception, are rigid flat feet due to tarsal coalition (fused segment of bone) in the back of the foot where freeing the blockage can restore function.
Stretching Exercises
Plantar Fasciitis stretches can be incorporated into a comprehensive treatment regime which may involve: ice, heel wedge support, taping, massage, muscle strengthening, orthotic inserts for shoes, topical anti inflammatory gel or oral medication and/or corticosteroid injections. If you suspect you may have Plantar Fasciitis seek accurate diagnosis and treatment from a health professional to ensure a correct diagnosis and reduce the likelihood of developing chronic foot pain. Treatment interventions may be provided by your Physical Therapist, Podiatrist and/or doctor.